Neuropathy Unmasked: Breaking Down the Misconceptions and Truths
Neuropathy is a condition that affects millions of people worldwide, yet it is often surrounded by confusion and misconceptions. Many individuals are unaware of the different types and causes of neuropathy, leading to assumptions that can hinder proper comprehension and treatment. This article aims to clarify what neuropathy truly is, breaking down the myths that often cloud this important health issue.
At its essence, neuropathy refers to injury or dysfunction of the nerves that can lead to a range of symptoms, including discomfort, numbness, and loss of strength. Various factors can contribute to neuropathy, ranging from high blood sugar and viral infections to injuries and autoimmune diseases. By exploring the underlying causes and addressing common misconceptions, we can gain a better picture of this complicated condition and how it impacts the lives of those affected.
What exactly is Peripheral Neuropathy?
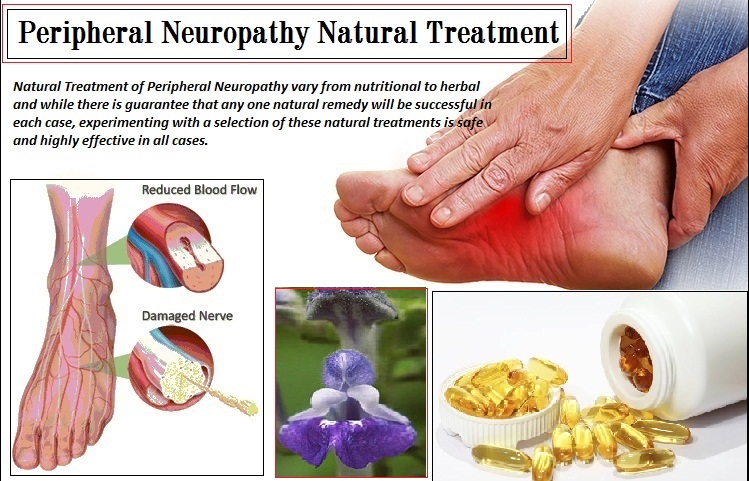
Peripheral neuropathy refers to a variety of issues that pertain to injury to the peripheral nervous system, which links the brain and spinal column to the remaining parts of the body. This damage can disrupt communication between the nervous system and various parts of the organism, leading to a range of manifestations. People with nerve damage often experience sensations such as pins and needles, numbness, or discomfort, particularly in the hands and feet.
There are a variety of causes of nerve damage, with diabetic conditions being one of the most common causes. Other factors can consist of viral or bacterial infections, exposure to poisons, hereditary disorders, and certain pharmaceuticals. The disorder can manifest in various forms, depending on what part of the neurological system is impacted. For example, motor neuropathy concerns the nerves responsible for muscle movement, while sensory neuropathy impacts the nerves responsible for transmitting sensory input.
Grasping nerve damage is vital for proper management and treatment. While it can be a persistent issue, many people with neuropathy can find relief through modifications to their lifestyle, medications, and rehabilitative therapy. Determining the underlying cause of nerve damage is essential for creating a tailored approach to treatment, making it vital for individuals experiencing symptoms to seek medical attention.
Common Myths About Peripheral Neuropathy
One common myth about neuropathy is that it solely affects elderly. Many individuals think that because neuropathy is frequently linked with age-related conditions like diabetes, it exclusively impacts the elderly. However, neuropathy can affect individuals of all ages, including children and young adults. Factors such as hereditary predisposition, autoimmune diseases, and exposure to toxins can lead to neuropathy regardless of a person's age.
Another prevalent misconception is that neuropathy is synonymous with pain. While pain is a frequent symptom of neuropathy, it is not the sole manifestation. Neuropathy can also manifest as numbness, tingling, weakness, or loss of coordination. Some individuals may experience no pain at all, leading to the false belief that they do not have neuropathy if they do not feel discomfort. It is important to recognize the range of symptoms linked with this condition.
Many people also believe that neuropathy is consistently a chronic condition. While some forms of neuropathy can indeed be chronic and progressive, there are cases where neuropathy can be treated successfully. Addressing underlying causes, such as controlling blood sugar levels in diabetic patients or avoiding harmful substances, can lead to improvements or even elimination of symptoms. Thus, it is important to approach neuropathy with an awareness that treatment options and outcomes differ widely.
Research-Backed Information on Peripheral Nerve Damage
Peripheral neuropathy refers to a spectrum of disorders that entail the presence of injury to the peripheral nerves, which can be caused by multiple causes such as diabetes, pathogens, autoimmune diseases, or contact with harmful substances. Diabetic nerve damage is considered one of the most common types of neuropathy, impacting up to one in two of people with a diabetic condition. This condition can present as loss of feeling, tingling, pain, and weakness, primarily in the upper extremities and feet. Understanding the underlying causes of neuropathy is vital for effective management and therapeutic approaches.
Recent studies indicate that early intervention can dramatically alter the progression of neuropathy. Efficient treatment often includes controlling blood sugar levels for diabetic patients, addressing micronutrient shortages, and incorporating healthier habits such as improved diet and increased physical activity. This proactive approach aims not only to reduce symptoms but also to prevent further nerve damage and consequences. Significantly, education about this condition can enable patients to recognize symptoms and request timely healthcare attention.
New treatments are emerging alongside standard methods. For instance, researchers are exploring the prospects of regenerative approaches, such as NGF therapies and neurostimulation methods. peripheral neuropathy treatment centers like alpha-lipoic acid and omega-3 fatty acids are also being investigated for their ability to protect nerves. As investigation proceeds, it is crucial to rely on evidence-based practices that provide the safest approaches for treating and comprehending neuropathy, in the end improving the quality of life for individuals who suffer from it.